RSPH discussed with vaccine experts what can we all do collectively as practitioners to improve vaccine uptake and reduce health inequalities
New data recently published by the NHS showed that vaccine coverage has decreased in 2022-2023. Once again, the UK has not met the World Health Organisation’s 95% coverage target, and some vaccines, such as the second dose of MMR, have reached the lowest levels since 2010-2011. In some areas of the country, coverage is as low as 56%, meaning that some children are now at risk of having measles, mumps, and rubella.
Vaccines are one of the most successful public health interventions in history and can be a powerful tool to reduce health inequalities. Deprived communities can benefit considerably from vaccine programmes, with research showing a higher reduction in mortality rates.
In recent research carried out by the RSPH, we asked children and young people (CYP) about their thoughts and experiences about vaccines. They told us they trust vaccines and think they are important to their health and would have a vaccine if it was convenient to them, for example, if they could have it at their school or close to home. However, CYP from Asian and black backgrounds have significantly different perceptions of vaccines, being more likely to be concerned about their safety, side effects and costs.
The RSPH discussed some of these issues with vaccine experts in a webinar. The goal was to think about what we could do collectively as practitioners and policymakers to improve uptake, reach underserved communities and better support the workforce. Below are the highlights of this discussion.
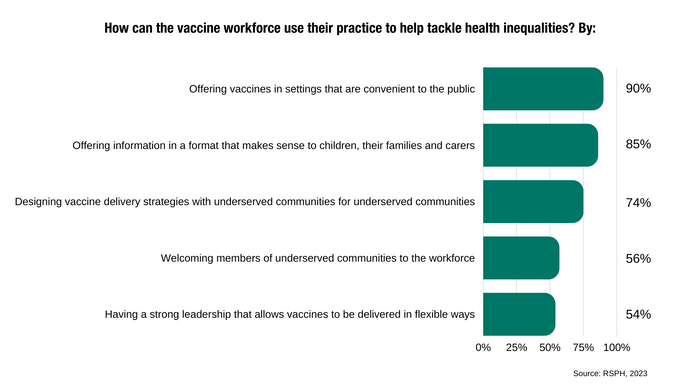
The importance of convenience. Vaccine services should be where people are, and go where people go. This includes being opportunistic and offering vaccines in non-traditional settings, such as A&E, supermarkets and shopping centres. Participants at the webinar also thought convenience was key, with 90% agreeing in a poll that the workforce could help tackle health inequalities by offering vaccines in settings that are convenient to the public.
Good communication is critical. Different vaccines prevent different diseases and have different side effects. Helping people access reliable information can address concerns, reassure them and empower them to make good decisions for their health. Also, some people don’t have a vaccine simply because they don’t know where to go, or what to do. Supporting them could make a real difference, and the more we talk about vaccines, the better. But as many say, communication is a two-way process. Listening to people and understanding what they need is crucial to optimise services and support communities.
The power of community. Communities know what they want and what they need from vaccine services. The ‘one size fits all’ approach does not work – especially when considering the histories and diversity of different communities. In other words, what works for one underserved community might not work for another. Different groups have different needs, and they require different solutions. Tailored approaches and the creation of bespoke delivery services can help us reach them more effectively. Listening and co-production are key.
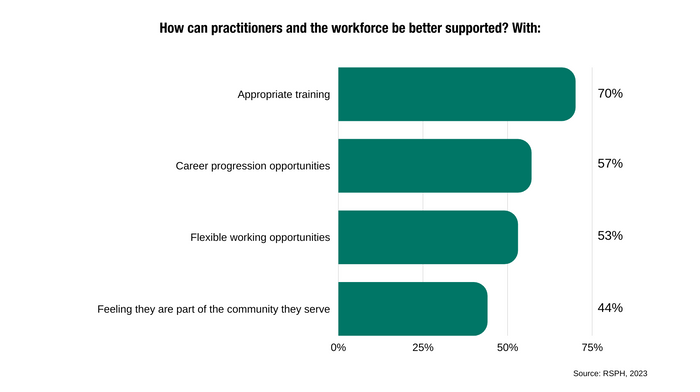
Supporting the workforce. The vaccination workforce does more than just offering vaccines: they reassure and provide information to members of the public, plan the services, assess individuals' health and collect data. Ensuring they have the training and materials they need to communicate properly with communities, valuing their work and offering career progression, creating CPD and upskilling opportunities would help alleviate pressures. Strong leadership and support for decision-making are important too. Proper funding and a joined-up approach to data and technology from local and regional services would also help streamline delivery and support this workforce. Participants of our webinar agreed in a pool that appropriate training is crucial to support people delivering vaccines.
The Covid-19 pandemic has shown that we can be creative and do things differently to deliver vaccines and achieve really strong results. Addressing inequalities can be complex and require careful consideration and an inclusive approach, and we should not be afraid to be led by the communities we work with. This includes developing bespoke vaccination plans for each one of the different underserved populations we work with. We must ask questions, understand and involve our groups, look for different platforms to send our message across, and use the power of communities as a catalyst to improve vaccine uptake. It is not a simple task, but we can all do it collectively and help improve uptake.
If you are a member of the RSPH, you can watch the recording of this webinar in our RSPH Sparks Debates section.



